Experiencing discomfort that starts in your jaw and seems to travel all the way up to your ear? You’re not alone. Many people report suffering from wisdom tooth pain spreading to ear, a symptom that can be incredibly distracting and debilitating. This common yet often misunderstood issue arises when your third molars, commonly known as wisdom teeth, encounter problems during their eruption. From dull aches to sharp, throbbing sensations, the unique anatomical connections in your head and face mean that issues originating with your wisdom teeth can readily manifest as ear pain, jaw stiffness, or even headaches.

It’s vital to understand why this phenomenon occurs, what other symptoms to look out for, and crucially, what steps you can take for relief. Ignoring the signs of wisdom tooth pain can lead to more serious complications, including infections that extend beyond your mouth. This comprehensive guide will delve into the intricate relationship between your wisdom teeth and your ears, providing practical advice, actionable home remedies, and clear guidance on when it’s time to seek professional dental care for that persistent ear discomfort.
Understanding the Connection: Why Wisdom Tooth Pain Spreads to Your Ear
The human head is a complex network of nerves, muscles, and bones, all intricately connected. When you experience wisdom tooth pain spreading to ear, it’s not simply an unfortunate coincidence; it’s a direct consequence of this anatomical proximity. Your wisdom teeth, situated at the very back of your jaw, share nerve pathways and muscle groups with your ears, temples, and jaw joint (temporomandibular joint, or TMJ).
One of the primary reasons for this referred pain is the trigeminal nerve. This major cranial nerve is responsible for transmitting sensations from your face, including your teeth, gums, and jaw, to your brain. When a wisdom tooth is impacted, infected, or erupting awkwardly, it can irritate branches of the trigeminal nerve. Because the same nerve also supplies sensation to parts of your ear, your brain can misinterpret the source of the pain, leading you to feel discomfort in your ear even though the problem originates in your mouth. This phenomenon, known as referred pain, is why an issue in one area can feel like it’s coming from another entirely.
Beyond nerve pathways, muscle tension also plays a significant role. When you have an uncomfortable wisdom tooth, you might unconsciously clench your jaw or alter your chewing patterns to avoid the pain. This can lead to tension in the muscles surrounding your jaw, neck, and even your inner ear, contributing to a dull ache or pressure. This muscular involvement can exacerbate ear pain from wisdom tooth issues, making it feel more pervasive and difficult to pinpoint.
The Anatomy of Referred Pain: From Jaw to Ear
To truly grasp why your wisdom tooth pain spreading to ear happens, it helps to visualize the shared structures. The temporomandibular joint (TMJ), located just in front of your ear, connects your jawbone to your skull. When wisdom teeth are causing problems, they can put stress on this joint. An impacted wisdom tooth, for example, might push against adjacent molars, altering your bite and causing strain on the TMJ. This strain can directly translate into discomfort that feels like an earache.
Furthermore, the Eustachian tube, which connects your middle ear to the back of your throat, helps regulate ear pressure. While not directly linked to wisdom teeth in the same way nerves are, severe inflammation or swelling in the back of the mouth due to a wisdom tooth infection could, in rare cases, subtly affect the pressure dynamics, leading to a feeling of fullness or mild pain in the ear. This makes it crucial to address the root cause, as untreated dental issues can cascade into broader discomfort.
It’s also worth considering the lymphatic system. Lymph nodes in your neck and under your jaw swell when fighting an infection. If a wisdom tooth is infected, these nodes will activate. Swollen lymph nodes, especially those located near the ear or jaw, can themselves cause localized tenderness and pain that might be mistaken for or contribute to an earache. This confluence of anatomical factors paints a clear picture of why your wisdom teeth can be a surprisingly common culprit behind unexplained ear discomfort.
Common Causes of Wisdom Tooth Pain Affecting the Ear
Understanding the reasons behind wisdom tooth pain spreading to ear is the first step toward effective relief. Several distinct issues with wisdom teeth can trigger this type of referred pain, ranging from the tooth’s eruption process itself to more serious infections. Recognizing these underlying causes is crucial for determining the appropriate course of action, whether it’s a simple home remedy or a necessary dental intervention.
Impacted Wisdom Teeth
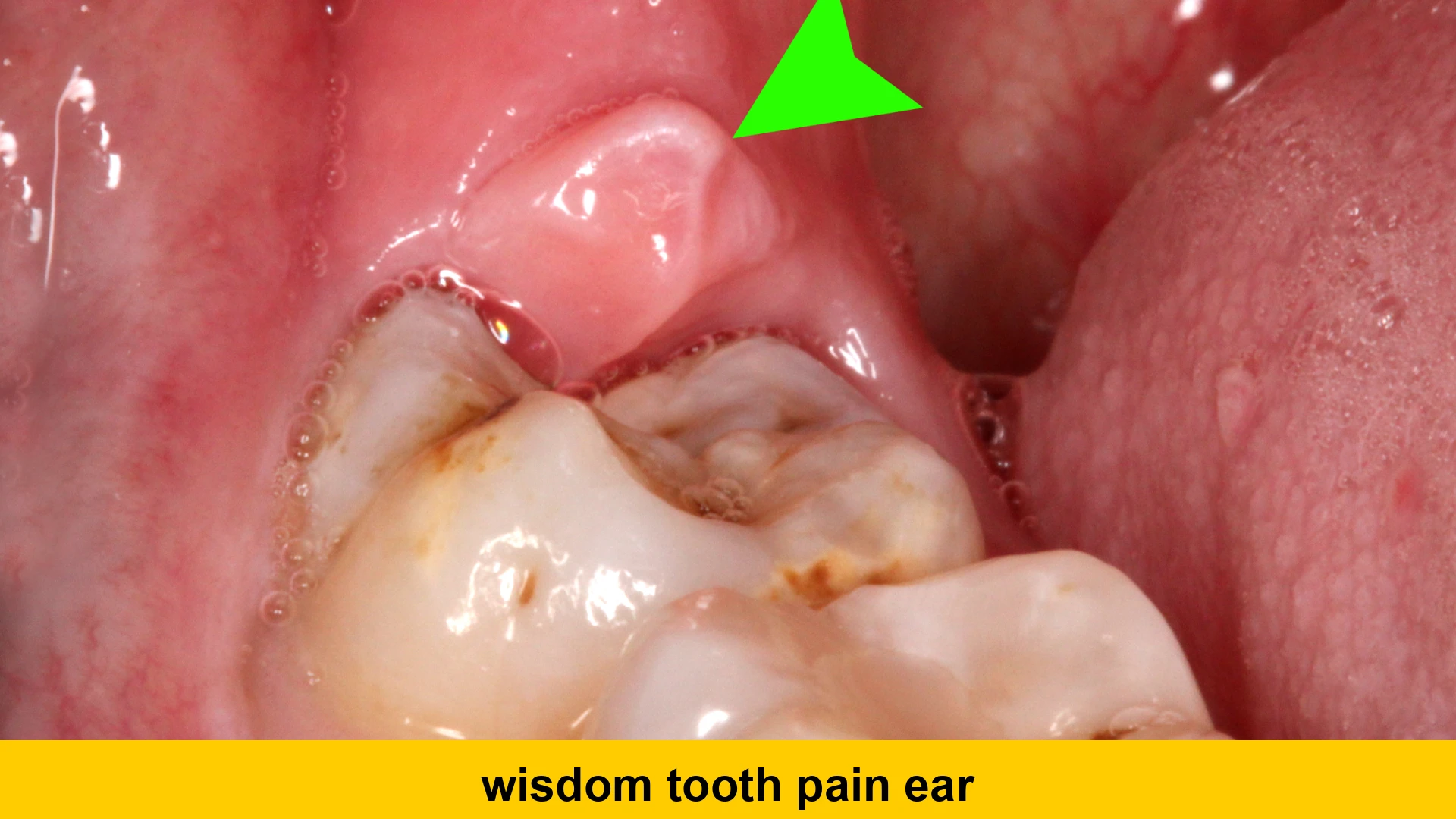
One of the most frequent causes of wisdom tooth pain spreading to ear is an impacted wisdom tooth. Impaction occurs when a wisdom tooth doesn’t have enough room to erupt properly and gets stuck partially or completely beneath the gum line, or against another tooth or bone. This can lead to a constant pressure sensation in the jaw that radiates upwards.
When a wisdom tooth is impacted, it often attempts to push through the gum tissue or against the roots of the adjacent molar. This persistent pressure can irritate the nerves in the area, including branches of the trigeminal nerve that extend to the ear. The discomfort can manifest as a dull ache, a sharp pain, or a throbbing sensation that feels distinctly like it’s originating in your ear. An impacted tooth can also cause the surrounding gum tissue to become swollen and tender, making it difficult to open your mouth fully, which further exacerbates referred pain to the jaw and ear.
Beyond just pressure, an impacted wisdom tooth can lead to the formation of a cyst around its crown, which can damage the surrounding bone and nerve structures. This less common but more severe complication can intensify the ear pain from wisdom tooth issues and necessitates immediate dental attention. Regular dental check-ups with X-rays can often identify impacted wisdom teeth before they cause significant discomfort, allowing for proactive treatment.
Pericoronitis: Infection of the Gum Tissue
Another prevalent cause of wisdom teeth causing earache is pericoronitis. This condition refers to the inflammation and infection of the gum tissue surrounding a partially erupted wisdom tooth. When a wisdom tooth only partially emerges, it creates a flap of gum tissue (an operculum) over the tooth’s surface. This flap can trap food particles, plaque, and bacteria, creating an ideal breeding ground for infection.
The infection can range from mild inflammation to a severe abscess. Symptoms often include localized pain, swelling, tenderness, and sometimes a foul taste in the mouth. As the infection progresses, the inflammation can spread to the jaw muscles, leading to stiffness and difficulty opening the mouth (trismus). The close proximity of the infection site to the ear, combined with the irritation of nerve endings and muscle tension, can result in significant sore ear wisdom teeth sensations.
In more severe cases of pericoronitis, the infection can spread to other areas of the face and neck, causing fever, chills, and widespread pain. If you suspect pericoronitis, especially with pus discharge or difficulty swallowing, it’s critical to see a dentist immediately. They can clean the area, prescribe antibiotics, and discuss options for removing the offending wisdom tooth to prevent recurrence.
Wisdom Tooth Decay or Cavities
While often associated with impaction or eruption issues, wisdom teeth are also susceptible to decay, just like any other tooth. Their location at the very back of the mouth makes them notoriously difficult to clean effectively, even with diligent brushing and flossing. This can lead to plaque buildup and, eventually, cavities. A deep cavity that reaches the tooth’s pulp (the innermost layer containing nerves and blood vessels) can cause significant pain.
When a wisdom tooth develops a cavity, particularly a large one, the resulting pain can be intense and radiate. The nerve irritation from decay or an infection within the tooth can extend along the trigeminal nerve pathways, leading to referred pain that feels like an earache. This kind of pain is often sharp, throbbing, and can be exacerbated by hot, cold, or sweet foods. It might also be accompanied by a sensitivity to biting pressure.
If left untreated, a cavity can lead to a dental abscess, a pocket of pus that forms at the tip of the tooth root due to a bacterial infection. An abscess can cause severe, persistent pain and swelling, and the infection can spread to surrounding bone and tissues, intensifying the wisdom tooth pain spreading to ear. Regular dental check-ups can help detect and treat cavities in wisdom teeth early, potentially preventing more severe symptoms and complications.
Cysts and Tumors (Less Common)
Though less common than impaction or infection, cysts and tumors can also develop around wisdom teeth, particularly impacted ones. A dentigerous cyst, for instance, is a fluid-filled sac that can form around the crown of an unerupted or impacted tooth. These cysts can grow quite large, putting pressure on the jawbone, adjacent teeth, and nerves.
The pressure exerted by a growing cyst can cause referred pain to the ear, along with jaw swelling and displacement of other teeth. While most cysts are benign, they can weaken the jawbone and, in rare cases, become infected or even transform into more aggressive lesions. Early detection through dental X-rays is vital, as larger cysts may require surgical removal to prevent further damage.
Similarly, benign tumors, though exceedingly rare, can also develop in the jawbone in association with wisdom teeth. These growths can also put pressure on surrounding structures and nerves, leading to symptoms like persistent jaw pain and ear discomfort. Any persistent, unexplained pain or swelling in the jaw area, especially if accompanied by difficulty moving the jaw or changes in bite, warrants immediate investigation by a dental professional.
Symptoms Beyond Ear Pain
While wisdom tooth pain spreading to ear is a clear indicator of a potential problem, it rarely occurs in isolation. It’s often part of a constellation of symptoms that point towards an issue with your wisdom teeth. Recognizing these additional signs can help you identify the problem more accurately and seek appropriate care before the situation escalates. Being aware of these accompanying symptoms is crucial for understanding the full scope of your discomfort.
Localized Oral Discomfort
Naturally, the most direct symptoms will manifest in your mouth itself. You might experience significant pain or tenderness at the very back of your jaw, precisely where your wisdom teeth are located. This pain can range from a dull ache to a sharp, throbbing sensation. It may be intermittent, flaring up when you chew or talk, or it could be a constant, nagging discomfort that makes it hard to focus. This localized pain is often the first indicator that something is amiss with your wisdom teeth.
Another common oral symptom is swelling and redness of the gums around the erupting or impacted wisdom tooth. This inflammation, known as pericoronitis, can be quite pronounced, making the gum tissue puffy and extremely sensitive to touch. You might even notice a flap of gum tissue partially covering the tooth. If an infection is present, there might be pus discharge, which can lead to a foul taste in your mouth or bad breath, signaling a bacterial problem.
Sensitivity to hot or cold temperatures, or pain when biting down, can also indicate a cavity in the wisdom tooth or damage to the adjacent molar. Sometimes, you might even feel a small, hard bump in the gum, which is the wisdom tooth beginning to push through. All these localized oral discomforts are strong clues that the discomfort radiating to your ear is indeed linked to your wisdom teeth.
Jaw and Facial Pain
The connection between your wisdom teeth and your jaw is undeniable, and problems in one often affect the other. Jaw pain wisdom teeth issues can cause is often a deep, aching sensation that can extend from the back of your jawline towards your chin or up your cheek. This pain can be particularly intense when you try to open your mouth wide, chew, or yawn.
Limited jaw movement, also known as trismus, is a very common symptom, especially with impacted wisdom teeth or infections. You might find it difficult or even impossible to open your mouth fully, making eating and speaking challenging. This stiffness is often due to inflammation and muscle spasms in the masseter and temporalis muscles, which are heavily involved in chewing and are close to the wisdom tooth area.
Facial swelling, particularly on one side of your face near the back of your jaw, is another clear sign of an underlying wisdom tooth problem, often indicative of an infection or severe inflammation. This swelling can make your face look noticeably asymmetrical and may be accompanied by tenderness to the touch. The referred ear pain causes this swelling and inflammation can create are substantial, making it difficult to discern the primary source of discomfort without professional help.
Other Related Symptoms
Beyond the oral and jaw-related issues, can wisdom tooth pain affect ear in other ways? Absolutely. Many individuals report headaches, particularly tension headaches that feel like they’re originating from the temples or spreading across the forehead. This is again due to the shared nerve pathways and muscle tension. The persistent strain from an erupting or impacted tooth can trigger these headaches, adding another layer of discomfort.
Sometimes, patients also experience a feeling of pressure or fullness in the ear, similar to what you might feel during a cold or with changes in altitude. This sensation can be directly linked to inflammation spreading to the Eustachian tube area or simply the referred sensation from nerve irritation. Swollen lymph nodes in the neck or under the jaw are another common accompanying symptom, especially if there’s an infection. These nodes feel like small, tender lumps and are your body’s way of fighting off bacteria.
In cases of severe infection, you might also develop a fever or general malaise, feeling tired and unwell. Difficulty swallowing (dysphagia) can also occur if the infection or swelling is significant enough to affect the muscles or tissues in the throat. Recognizing this full spectrum of potential symptoms is essential for anyone dealing with wisdom tooth pain spreading to ear, as it helps paint a complete picture for your dental professional.
When to Seek Professional Help
While some minor wisdom tooth discomfort can be managed at home, there are critical signs that indicate you need to see a dentist or oral surgeon immediately. Ignoring severe or persistent symptoms of wisdom tooth pain spreading to ear can lead to serious complications, including widespread infection, damage to adjacent teeth, or even systemic health issues. Knowing when to escalate your concerns is crucial for your oral and overall health.
Signs of Infection
An infection is perhaps the most urgent reason to seek professional dental care. If you notice any of the following symptoms alongside your wisdom tooth pain spreading to ear, it’s time to call your dentist without delay:
- Fever and Chills: A fever indicates your body is fighting a significant infection.
- Pus Discharge: Seeing or tasting pus from the gums around your wisdom tooth is a clear sign of infection (pericoronitis or abscess).
- Severe Swelling: Noticeable swelling in your jaw, cheek, or neck that is rapidly worsening.
- Difficulty Swallowing or Breathing: If swelling from an infection spreads to your throat, it can impede your ability to swallow or, in extreme cases, breathe. This is a medical emergency.
- Intense, Throbbing Pain: Pain that is severe, constant, and throbbing, especially if it wakes you up at night.
- Foul Taste or Odor: A persistent bad taste in your mouth or bad breath that doesn’t go away with brushing can indicate an infection.
Untreated dental infections can spread to other parts of your head and neck, potentially leading to serious conditions like cellulitis or even sepsis. Do not delay seeking help if you suspect an infection. Your dentist can prescribe antibiotics and plan for the removal of the problematic tooth to prevent recurrence.
Persistent or Worsening Pain
If your wisdom tooth pain spreading to ear doesn’t improve after a few days of home remedies, or if it progressively worsens, it’s a strong signal that professional intervention is needed. Persistent pain, even if not accompanied by overt signs of infection, can indicate an impacted tooth causing ongoing pressure, nerve irritation, or developing decay that requires treatment.
Sometimes, the pain may start as a mild ache and gradually intensify, becoming more difficult to manage with over-the-counter pain relievers. This escalation suggests that the underlying issue is progressing. Similarly, if your jaw pain, stiffness, or inability to open your mouth wide continues for more than a few days, it’s essential to get it checked. Prolonged strain on the temporomandibular joint (TMJ) can lead to chronic TMJ disorder if the wisdom tooth issue isn’t resolved.
A dentist can perform a thorough examination, including X-rays, to accurately diagnose the problem. They can assess the position of your wisdom teeth, look for signs of impaction, decay, or infection, and determine the most effective course of treatment. Don’t wait until the pain becomes unbearable; proactive care can prevent further complications and provide faster relief from why does my wisdom tooth cause ear pain.
Other Concerning Symptoms
Beyond infection and escalating pain, there are other symptoms that warrant a visit to the dentist:
- Limited Jaw Opening (Trismus): If you can’t open your mouth fully, it can be a sign of significant inflammation or muscle spasm caused by your wisdom tooth.
- Difficulty Chewing or Biting: If chewing is painful or impossible, it impacts your nutrition and overall well-being.
- Bleeding Gums: While some minor bleeding can occur with brushing, persistent or excessive bleeding around the wisdom tooth can indicate inflammation or infection.
- Unexplained Headaches: If you’re experiencing frequent or severe headaches that seem to coincide with your wisdom tooth discomfort and referred ear pain, a dental evaluation can rule out the dental origin.
- Cyst or Tumor Formation: Although rare, a growing bump or lump in the jaw area that feels firm and doesn’t go away should be examined immediately.
Ultimately, trust your instincts. If something feels genuinely wrong, or if your quality of life is significantly impacted by can an impacted wisdom tooth cause ear pain, don’t hesitate to seek a professional opinion. Early diagnosis and treatment are always better for preventing long-term damage and ensuring a quicker recovery from such discomfort.
Diagnosis: What to Expect at the Dentist
When you visit your dentist concerning wisdom tooth pain spreading to ear, they will conduct a thorough examination to pinpoint the exact cause of your discomfort. A precise diagnosis is essential for developing an effective treatment plan, as different wisdom tooth issues require different interventions. Knowing what to expect during your appointment can help alleviate any anxiety and prepare you for the process.
Oral Examination and X-rays
Your visit will typically begin with a detailed discussion of your symptoms. Be prepared to describe the nature of your pain (sharp, dull, throbbing), its location, how long it’s been present, and any factors that seem to worsen or alleviate it, including the ear pain from wisdom tooth issues. Your dentist will also ask about your overall health history and any medications you are taking.
Next, a comprehensive oral examination will be performed. Your dentist will visually inspect the area around your wisdom teeth, looking for signs of swelling, redness, pus, or decay. They will gently probe the gum tissue and tooth to check for tenderness and assess the level of inflammation. They will also evaluate your bite and jaw movement, checking for any limitations or pain when you open and close your mouth.
One of the most crucial diagnostic tools is dental X-rays. Periapical X-rays provide detailed images of individual teeth, while a panoramic X-ray captures a full view of your entire mouth, including all teeth, jaws, and surrounding structures. These X-rays are invaluable for:
- Detecting impacted wisdom teeth and their exact position relative to adjacent teeth and nerves.
- Identifying signs of decay, especially in wisdom teeth that are difficult to see visually.
- Checking for the presence of cysts or tumors around the wisdom teeth.
- Assessing bone health and any damage to surrounding structures.
X-rays provide the dentist with a clear picture of what’s happening beneath the gum line, confirming if your is ear pain a symptom of wisdom tooth eruption or other issues. In some complex cases, a 3D cone-beam computed tomography (CBCT) scan might be recommended to get an even more detailed view, particularly if the wisdom tooth is very close to vital structures like nerves or the sinus cavity.
Differentiating from Other Causes of Ear Pain
It’s important for your dentist to confirm that the ear pain is indeed originating from your wisdom tooth and not from another source. Ear pain can stem from various causes, including ear infections, temporomandibular joint (TMJ) disorders not directly related to wisdom teeth, sinus infections, or even problems with other teeth. Your dentist is trained to differentiate these conditions.
During the examination, your dentist will carefully evaluate your TMJ for tenderness, clicking sounds, or limited movement. They might ask you to perform certain jaw movements to assess its function. While jaw pain wisdom teeth issues can cause TMJ symptoms, an independent TMJ disorder might require a different treatment approach. They will also look for signs of other dental problems that could be referring pain to the ear.
If the dental examination and X-rays don’t reveal a clear dental cause for your ear pain, your dentist might recommend consulting with an ear, nose, and throat (ENT) specialist or your primary care physician to rule out non-dental origins. However, given the commonality of wisdom tooth pain spreading to ear, a thorough dental assessment is almost always the first and most critical step in identifying the true source of your discomfort. This systematic approach ensures that you receive the correct diagnosis and the most appropriate treatment, getting you closer to relief from your uncomfortable symptoms.
How to Relieve Wisdom Tooth Pain and Ear Discomfort at Home
While professional dental intervention is often necessary for long-term resolution of wisdom tooth pain spreading to ear, there are several effective home remedies and over-the-counter solutions that can provide temporary relief from discomfort. These methods can help manage pain and inflammation until you can see a dentist or as a supportive measure post-treatment. Always remember that home remedies are not a substitute for professional dental care, especially if you suspect an infection.
Over-the-Counter Pain Relief
For immediate relief from both tooth and referred ear pain, over-the-counter (OTC) pain relievers are your first line of defense. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) or naproxen (Aleve) are particularly effective because they reduce both pain and inflammation. Follow the dosage instructions on the packaging carefully.
Acetaminophen (Tylenol) can also alleviate pain, though it doesn’t reduce inflammation as effectively as NSAIDs. You might find a combination approach, alternating between ibuprofen and acetaminophen (if safe for you), provides more comprehensive pain control, especially for significant wisdom teeth causing earache. Always check for contraindications with your existing medications or health conditions before starting any new OTC pain regimen.
Topical pain relief can also be helpful. Gels or liquids containing benzocaine (like Orajel) can be applied directly to the sore gum around the wisdom tooth for temporary numbing. Ensure you apply it carefully to avoid numbing your tongue or throat, and use it sparingly, as its effects are short-lived. These can offer quick but transient relief from localized pain and may slightly diminish the sensation of ear pain from wisdom tooth.
Warm Saltwater Rinses
A simple yet incredibly effective home remedy for oral pain and inflammation is a warm saltwater rinse. Saltwater acts as a natural disinfectant, helping to reduce bacteria in the mouth and clean the area around the wisdom tooth. It can also help soothe inflamed gum tissue and reduce swelling, which indirectly can alleviate wisdom tooth pain spreading to ear.
To prepare a saltwater rinse, dissolve half a teaspoon of salt in a glass of warm water. Swish the solution around your mouth for about 30-60 seconds, paying particular attention to the affected area, before spitting it out. Repeat this process 2-3 times a day, especially after meals. The warmth can be comforting, and the antiseptic properties can help keep a potential infection at bay, offering some relief from a sore ear wisdom teeth causes.
This method is particularly beneficial if food particles are trapped under a gum flap around a partially erupted wisdom tooth, as the rinse can help dislodge them and clean the area, reducing the risk of pericoronitis. Regular rinsing can significantly improve oral hygiene when you’re struggling to brush the back of your mouth due to pain or limited opening.
Cold Compresses
Applying a cold compress to the outside of your jaw can help reduce swelling and numb the painful area, offering temporary relief from both localized tooth pain and referred wisdom tooth pain spreading to ear. Cold therapy works by constricting blood vessels, which in turn reduces inflammation and dulls nerve signals.
To use a cold compress, wrap an ice pack or a bag of frozen vegetables in a thin cloth to protect your skin. Apply it to the outside of your cheek, directly over the area of the painful wisdom tooth, for 15-20 minutes at a time. You can repeat this every few hours. This is especially helpful if you have noticeable facial swelling. The cooling sensation can also distract from the throbbing pain, making it easier to manage your discomfort.
While cold compresses are excellent for acute pain and swelling, some people find warm compresses more comforting for muscle stiffness or tension. You can alternate between cold and warm if you find both beneficial, but always prioritize cold for immediate swelling reduction. This simple, actionable step can provide significant short-term relief for what to do for wisdom tooth pain radiating to ear.
Oral Hygiene and Dietary Adjustments
Maintaining excellent oral hygiene is paramount, even when experiencing pain. Gently brush the area around your wisdom tooth to remove food debris and plaque, which can exacerbate inflammation and infection. If brushing is too painful, continue with saltwater rinses and consider using a soft-bristled brush or an interdental cleaner to carefully clean as much as possible.
Making temporary dietary adjustments can also reduce irritation. Stick to soft foods that require minimal chewing, such as soups, yogurts, mashed potatoes, and smoothies. Avoid hard, crunchy, or sticky foods that could get lodged around the wisdom tooth or put undue pressure on your jaw. Also, avoid extremely hot or cold foods and beverages if they trigger sensitivity.
Refrain from consuming sugary drinks, alcohol, and tobacco products, as these can irritate inflamed tissues and hinder the healing process. Staying hydrated with plain water is always a good idea. By reducing strain on your jaw and keeping the area as clean as possible, you can mitigate some of the discomfort associated with how to relieve wisdom tooth ear pain at home and prevent further complications while awaiting professional dental care.
Medical and Dental Treatments for Relief
While home remedies can offer temporary respite, addressing the underlying cause of wisdom tooth pain spreading to ear often requires professional medical or dental intervention. Depending on the diagnosis, your dentist or oral surgeon will recommend a specific course of treatment designed to alleviate pain, resolve infection, and prevent future complications. Understanding these options is key to making informed decisions about your oral health.
Antibiotics for Infection
If your dentist determines that the ear pain from wisdom tooth is due to an infection, such as pericoronitis or a dental abscess, antibiotics will likely be prescribed. Common antibiotics include penicillin-based drugs (like amoxicillin) or clindamycin for those with penicillin allergies. It is crucial to take the entire course of antibiotics exactly as prescribed, even if your symptoms improve before you finish the medication. Stopping early can lead to the infection recurring and potentially becoming more resistant to treatment.
Antibiotics work by killing the bacteria causing the infection or inhibiting their growth, thereby reducing inflammation, swelling, and pain. While antibiotics can effectively manage the infection, they do not resolve the underlying issue, such as an impacted tooth or a deep cavity. Therefore, antibiotic treatment is often a preparatory step before other definitive treatments, like tooth extraction. Addressing the infection first makes subsequent procedures safer and more successful, paving the way for lasting relief from wisdom tooth infection causing ear discomfort.
Wisdom Tooth Extraction
In many cases, the definitive solution for recurrent or severe wisdom tooth pain spreading to ear is extraction of the problematic tooth. This is especially true for impacted wisdom teeth, those causing pericoronitis, or those that are severely decayed and cannot be restored. Your dentist or oral surgeon will assess the position of the tooth, its roots, and its proximity to nerves and sinuses to determine the best extraction method.
Wisdom tooth extraction can be a straightforward procedure for fully erupted teeth or a more complex surgical extraction for impacted teeth. During the procedure, local anesthesia is used to numb the area, and sometimes sedation (oral, IV, or nitrous oxide) is offered for patient comfort. The dentist or oral surgeon will carefully remove the tooth, and sutures may be placed to help the gum heal.
Extraction eliminates the source of the problem, providing long-term relief from pain, swelling, and referred discomfort. While there is a recovery period, the benefits of removing a problematic wisdom tooth usually far outweigh the temporary post-operative discomfort. It’s the most common and effective treatment for persistent can wisdom tooth pain affect ear issues linked to these molars. For more information on wisdom tooth care and extractions, you can consult Mayo Clinic’s guide on wisdom teeth.
Other Dental Interventions
In some less common scenarios, alternatives to full extraction or additional procedures might be considered:
- Operculectomy: If pericoronitis is a recurring issue and the wisdom tooth is expected to fully erupt eventually, a dentist might remove the overlying gum flap (operculum) to prevent food trapping and reinfection. This can provide relief from sore ear wisdom teeth cause by gum inflammation.
- Dental Fillings or Root Canal: If the wisdom tooth has a cavity that is not too deep and the tooth is otherwise healthy and well-positioned, a dental filling might be sufficient. If the decay is extensive and reaches the pulp, a root canal might be performed to save the tooth, though this is less common for wisdom teeth due to their position and often limited long-term prognosis.
- Orthodontic Treatment: In very rare cases, if space is the primary issue and extraction is not preferred, orthodontic intervention might be discussed to create room, but this is usually a long-term plan and not an immediate solution for acute pain.
Your dentist will discuss all viable options with you, explaining the pros and cons of each, to determine the most appropriate and effective treatment for your specific situation. The ultimate goal is to eliminate your pain, resolve any infection, and prevent future occurrences of wisdom tooth pain spreading to ear, ensuring your comfort and oral health.
Post-Extraction Care and Ear Pain Relief
Undergoing a wisdom tooth extraction is a common procedure, and while it ultimately resolves the source of your wisdom tooth pain spreading to ear, it’s important to be prepared for the recovery period. Post-operative care is crucial for minimizing discomfort, preventing complications, and ensuring a smooth healing process. Even after extraction, some referred ear pain might linger temporarily as your body heals and inflammation subsides.
Managing Post-Operative Discomfort
Immediately after wisdom tooth extraction, you can expect some degree of pain, swelling, and sometimes even bruising. Your oral surgeon or dentist will provide detailed post-operative instructions, which typically include:
- Pain Medication: You will likely be prescribed stronger pain medication or advised to continue with over-the-counter NSAIDs (like ibuprofen) to manage the discomfort. Take these as directed and before the pain becomes severe.
- Cold Compresses: Apply an ice pack to the outside of your cheek for 15-20 minutes at a time, every hour or two, during the first 24-48 hours. This helps to reduce swelling and can also provide relief for any lingering wisdom tooth extraction ear pain relief.
- Soft Diet: Stick to soft foods for several days to a week. Avoid chewing on the extraction site and refrain from hard, crunchy, or sticky foods that could irritate the wound.
- Oral Hygiene: While you shouldn’t rinse vigorously, your dentist will likely recommend gentle saltwater rinses (after the first 24 hours) to keep the area clean and aid healing. Avoid spitting forcefully or using straws, as this can dislodge the blood clot and lead to a painful condition called dry socket.
It’s normal to experience some jaw stiffness or soreness for a few days, which can contribute to a sensation of ear discomfort. Gentle jaw exercises, as advised by your dentist, can help restore normal function. If you find your wisdom tooth pain spreading to ear persists or worsens significantly after the initial recovery period, or if you develop new symptoms, contact your dental professional immediately.
When to Be Concerned During Recovery
While some discomfort is expected, certain post-operative symptoms warrant immediate attention. These can indicate a complication, such as infection or dry socket:
- Increased or Severe Pain: If your pain suddenly worsens after a few days, or if the pain medication is ineffective, it could be a sign of dry socket (when the blood clot at the extraction site dislodges) or an infection. Dry socket pain often radiates to the ear.
- Persistent Swelling: While initial swelling is normal, if it increases after 2-3 days, or if you develop new swelling, it could indicate an infection.
- Fever: A fever after the first day or two post-surgery suggests an infection.
- Pus or Foul Odor: Any discharge of pus or a foul taste/smell from the extraction site is a clear sign of infection.
- Difficulty Swallowing or Breathing: These are serious symptoms that require immediate medical attention.
Always follow your oral surgeon’s instructions precisely. They are your best resource for guiding you through a smooth recovery and addressing any concerns about wisdom tooth extraction ear pain relief. By taking proper care of yourself after the procedure, you’ll minimize discomfort and promote quick healing, allowing you to return to normal activities without the nagging pain in your ear and jaw.
Preventing Future Wisdom Tooth Pain
While some wisdom tooth issues are unavoidable, particularly genetic predisposition to impaction, there are proactive steps you can take to minimize your risk of developing future wisdom tooth pain spreading to ear and other related complications. Prevention largely revolves around maintaining excellent oral hygiene and regular dental check-ups, ensuring any potential problems are identified and addressed early.
Regular Dental Check-ups and X-rays
The most crucial preventive measure is regular visits to your dentist. For most adults, this means a check-up and cleaning every six months. During these appointments, your dentist can monitor the development and position of your wisdom teeth, even if they haven’t erupted yet. X-rays are particularly vital in this regard, as they allow your dentist to:
- Assess Impaction: X-rays reveal if wisdom teeth are impacted, at what angle, and if they are likely to cause problems in the future. Early detection of impaction allows for planned extraction before pain or infection sets in.
- Detect Cysts/Tumors: Although rare, X-rays can identify the presence of cysts or tumors associated with impacted teeth, allowing for early intervention.
- Monitor Eruption: For teeth that are erupting, X-rays show if there is enough space and if the eruption path is normal.
Your dentist can also detect early signs of decay in wisdom teeth, which are often hard to clean, or identify pericoronitis before it becomes a full-blown infection causing wisdom teeth causing earache. Discussing your wisdom teeth with your dentist, especially if you experience any mild, intermittent discomfort, can help you make informed decisions about their management.
Optimal Oral Hygiene Practices
While your wisdom teeth are in your mouth, whether fully erupted or partially, meticulous oral hygiene is essential to prevent decay and infection, both of which can lead to wisdom tooth pain spreading to ear. Their location at the back of the mouth makes them challenging to clean, but consistent effort can make a significant difference.
- Thorough Brushing: Use a soft-bristled toothbrush and pay extra attention to the very back of your mouth. Angle the brush to reach all surfaces of the wisdom teeth and the gum line. Consider an electric toothbrush, which can often clean more effectively in hard-to-reach areas.
- Daily Flossing: Flossing is critical for removing food particles and plaque from between teeth and under the gum line, especially around partially erupted wisdom teeth. If flossing is difficult, consider using interdental brushes or a water flosser.
- Antiseptic Mouthwash: Rinsing with an antiseptic mouthwash can help reduce bacteria in your mouth and further clean areas that brushing and flossing might miss. This is particularly helpful in preventing pericoronitis around erupting teeth.
- Warm Saltwater Rinses: Even if you’re not experiencing acute pain, periodic warm saltwater rinses can help maintain a clean and healthy oral environment, reducing inflammation and bacteria, thus minimizing the chances of wisdom tooth infection causing ear discomfort.
By making these hygiene practices a consistent part of your daily routine, you can significantly reduce the risk of developing problems with your wisdom teeth. While extraction is often the recommended solution for problematic wisdom teeth, these preventive measures can help you avoid complications and manage discomfort until a definitive treatment plan is established, providing long-term relief from why does my wisdom tooth cause ear pain and associated discomfort.
Differentiating Wisdom Tooth Ear Pain from Other Causes
While this article focuses on wisdom tooth pain spreading to ear, it’s important to acknowledge that ear pain can stem from numerous other sources. Understanding the distinguishing characteristics can help you and your healthcare provider narrow down the cause, especially if your dental examination doesn’t reveal a clear wisdom tooth problem. Misdiagnosing the source of ear pain can lead to delayed or ineffective treatment.
Ear Infections (Otitis Media/Externa)
Ear infections are a very common cause of ear pain, particularly in children but also affecting adults. These infections are primarily located within the ear canal (otitis externa, or ‘swimmer’s ear’) or behind the eardrum in the middle ear (otitis media). While the pain can sometimes feel similar to referred dental pain, there are usually key differences:
- Location: Ear infection pain is typically localized within the ear itself, often deep inside. Dental pain, even when referred, usually has a stronger focal point at the back of the jaw.
- Associated Symptoms: Ear infections often come with a feeling of fullness in the ear, muffled hearing, drainage from the ear canal, or even fever and general malaise. These are less common with purely dental-related ear pain unless a significant dental infection has spread.
- Trigger Factors: Ear infection pain is often constant, whereas referred pain from a wisdom tooth might be exacerbated by chewing, jaw movement, or pressure on the jaw area.
If your primary symptoms are within the ear, especially if accompanied by hearing changes or discharge, it’s more likely an ear infection requiring an ENT or primary care doctor’s attention rather than wisdom tooth pain spreading to ear.
Temporomandibular Joint (TMJ) Disorders
The temporomandibular joint (TMJ) connects your jawbone to your skull and is located just in front of your ear. Dysfunction in this joint can cause significant pain that is often mistaken for or contributes to ear pain. TMJ disorders (TMD) can result from various factors, including teeth grinding (bruxism), jaw clenching, injury, or arthritis.
- Location: TMD pain is typically felt directly in front of the ear, often accompanied by pain in the jaw muscles, temples, and neck. It can mimic ear pain causes stemming from wisdom teeth.
- Jaw Symptoms: Key indicators of TMD include clicking, popping, or grinding sounds when opening or closing your mouth, limited jaw movement, and tenderness in the jaw muscles. These symptoms are also common with wisdom tooth issues, which is why differentiation can be tricky.
- Triggers: TMD pain is often aggravated by chewing hard foods, wide yawning, or excessive talking. Stress can also exacerbate clenching and grinding, leading to TMD symptoms.
While an impacted wisdom tooth can sometimes cause or worsen TMD symptoms by altering your bite or creating muscle tension, TMD can also exist independently. Your dentist will carefully examine your jaw and may perform specific tests to differentiate if jaw pain wisdom teeth issues are the primary cause or if a separate TMJ disorder is at play.
Other Dental Problems
It’s also possible for other dental issues, not specifically related to wisdom teeth, to cause referred ear pain. For instance:
- Deep Cavities in Other Molars: A large cavity or infection in one of your regular molars (not just wisdom teeth) can irritate nerve pathways and cause referred pain to the jaw and ear.
- Cracked Tooth Syndrome: A cracked tooth, which might not be visible, can cause intermittent pain, especially when chewing, which can radiate.
- Dental Abscess: An abscess on any tooth can lead to significant pain, swelling, and referred discomfort.
A comprehensive dental examination, including X-rays, is crucial to rule out these possibilities. Your dentist’s expertise in diagnosing oral pathology will ensure that the correct source of your discomfort is identified, leading to the most appropriate treatment and effective relief from any type of ear pain causes originating from your dental health.
Conclusion
The experience of wisdom tooth pain spreading to ear is a clear signal from your body that something is amiss with your third molars. From impacted teeth exerting pressure on sensitive nerves to infections like pericoronitis inflaming surrounding tissues, the close anatomical relationship between your wisdom teeth, jaw, and ear means discomfort can easily radiate. While home remedies such as warm saltwater rinses and over-the-counter pain relievers can offer temporary relief, they are not a substitute for professional dental care.
It’s crucial to pay attention to accompanying symptoms like jaw stiffness, facial swelling, or fever, as these can indicate an escalating infection that requires immediate attention. A visit to your dentist, complete with a thorough oral examination and diagnostic X-rays, is the most effective way to accurately determine the cause of your discomfort and rule out other potential sources of ear pain. Whether the solution involves antibiotics for an infection or a wisdom tooth extraction to resolve chronic issues, timely intervention is key to preventing further complications and achieving lasting comfort. Don’t let the nagging pain of can wisdom tooth pain affect ear diminish your quality of life; seek professional advice and take proactive steps towards a healthier, pain-free smile.